Asthma
Asthma in Infants
Asthma can start at any age, even in infancy. But asthma in infants can look different than asthma in children and adults. This can also make it harder to diagnose. By knowing how to manage asthma and spot symptoms, you can successfully manage your baby’s asthma.
The signs and symptoms of asthma in a baby or toddler include:
- Fast breathing
- Working harder to breathe (nostrils flaring, skin is sucking in around and between ribs or above the sternum, or exaggerated belly movement)
- Panting with normal activities such as playing
- Wheezing (a whistling sound)
- Persistent coughing
- Difficulty sucking or eating
- Tiredness, not interested in normal or favorite activities
- Cyanosis, a tissue color change on mucus membranes (tongue, lips, and around the eyes) and fingertips or nail beds – the color appears grayish or whitish on darker skin tones and bluish on lighter skin tones
Closed Accordion
What Causes Asthma in Infants and Toddlers?
We still do not know what causes some people to get asthma. If a child has a family history of asthma or allergies, a specific allergy, or had a mother who smoked during pregnancy, they have a higher chance of getting asthma early in life.
A respiratory virus, an illness that occurs in the lungs, is one of the most common causes of asthma symptoms in children 5 years old and younger. Although both adults and children experience respiratory infections, children have more of them. Some preschool children get viral infections often. At least half of children with asthma show some sign of it before the age of 5. Viruses are the most common cause of acute asthma episodes in infants 6 months old or younger.
How Is Asthma in Infants and Toddlers Different Than Adult Asthma?
Infants and toddlers have much smaller airways than older children and adults. In fact, these airways are so small that even small blockages caused by viral infections, tight airways, or mucus can make breathing difficult for the child.
Is It Asthma or Something Else?
Asthma symptoms can look like symptoms of other illnesses or diseases. The following may have symptoms similar to asthma:
- Bronchiolitis
- Croup
- Acid reflux
- Pneumonia
- Upper respiratory viruses
- Aspiration
- Inhaled object
- Epiglottis
- Cystic fibrosis
- Birth defects
How Is Asthma Diagnosed in Infants and Toddlers?
It is hard to diagnose asthma in infants and toddlers. Since they are not able to talk well, they cannot describe how they are feeling. A fussy baby could mean many things. Toddlers and preschoolers are often active, even with chest tightness or trouble breathing.
Parents should give the following information to their child’s doctor:
- Family history of asthma or allergies
- The child’s behavior
- Breathing symptom patterns (nighttime vs. daytime, with activity or at rest, response to any medicines, harder to breath out vs. in)
- Potential triggers and responses to foods or possible allergy triggers
Lung function tests – often used to make a complete asthma diagnosis – are hard to do with young children. Instead, the doctor may see how the child responds to medicines to improve breathing. The doctor may order blood tests, allergy testing, and X-rays to get more information.
Using this information, the doctor can make the best diagnosis. Parents may need to take their child to a pediatric allergist or pulmonologist (lung specialist) for special testing or treatment.
What Is the Treatment for Asthma in Infants and Toddlers?
Infants or toddlers can use most asthma medicines used for older children and adults. The dosage may be lower and the way the child takes it is different. Inhaled medicines work fast to make symptoms better and produce few side effects.
Medicines used to treat asthma symptoms in infants and toddlers are usually given in inhaled forms. Infants are usually treated with medicine given by a nebulizer or with an inhaler using a spacer with a mask. A nebulizer (sometimes called a “breathing machine”) is a small machine that uses forced air to create a medicine mist for the baby to breathe through a small face mask. Nebulizer treatments take about 10 minutes. A spacer is a small tube, or aerochamber, which holds the medicine released by the inhaler fitted into it. The inhaler/spacer device allows children to breathe in the medicine. Medicines given via inhaler with a spacer and mask work just as well as medicines given by a nebulizer. In some cases, the child might tolerate the inhaler with spacer and mask better.
Asthma is treated with several different medicines. Bronchodilators are quick-relief medicines (also called “rescue” or “reliever” medicines) that open up airways to relieve sudden symptoms. Controller medicines like inhaled corticosteroids, long-acting bronchodilators, combination medicines, or leukotriene modifiers taken for maintenance are used to calm swelling in the airways and keep asthma symptoms low. Many people with asthma, including infants and toddlers, are given a mix of medicines depending on how severe and how often they have symptoms. Work with your child’s doctors to develop an asthma care management plan.
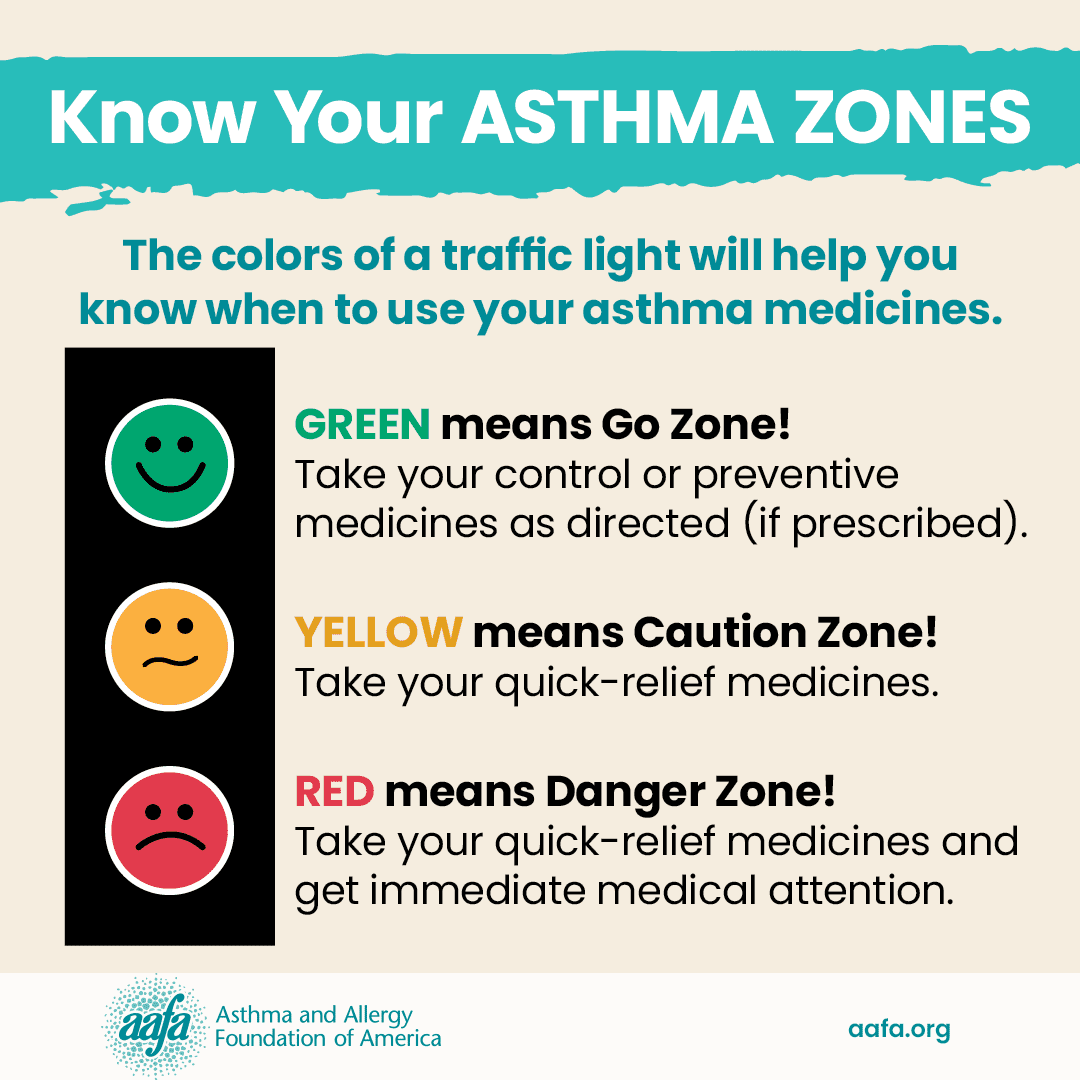
This plan should include an Asthma Action Plan. An Asthma Action Plan is a document that tells you how to manage your child’s asthma according to their symptoms. If your child does not have an Asthma Action Plan, work with their doctor to create one. Keep a copy close by at all times, and share with other people who care for your child, such as family, friends, and child care providers.
What Can I Do to Manage My Child’s Asthma?
- Learn the warning signs for increasing asthma in infants and toddlers. Know your child’s particular asthma symptom “pattern.”
- Develop an Asthma Action Plan with your child’s doctor. Make sure the plan has a course of action to follow if asthma symptoms get worse. Understand when your child needs emergency care.
- Follow your child’s Asthma Action Plan every day! Don’t change the plan until you consult your child’s doctor. Even if your child’s symptoms are gone, stick with the plan until you discuss changes with the doctor.
- Teach your toddler or preschooler to tell you when they are not feeling well.
- Work out an emergency plan of action to follow if your child has a serious asthma episode. What hospital will you use? (Be sure your doctor uses that hospital and it is in your health care plan.) Who will take care of your other children? How does your medical coverage provide for emergency care?
What Can I Do to Reduce Asthma Symptoms?
- Learn your child’s triggers.
- Allergens like dust mites, pets, pests, molds, and pollen can play a role in some children’s asthma. Discuss with your child’s doctor whether an evaluation by an allergist may be helpful.
- Follow your asthma management plan and give the medicines prescribed by your child’s doctor.
- Avoid smoking near your child.
Can a Child Outgrow Asthma?
Medical Review December 2021 by Michael Pistiner, MD, MMSc, and Mitchell Grayson, MD