Asthma
COVID-19 (Coronavirus Disease), Asthma, and Allergies
COVID-19 is a disease caused by a virus called SARS-CoV-2 (a type of coronavirus). It causes respiratory symptoms, but it can also affect other parts of your body. Some people may have long-term symptoms called “Long COVID.”
The COVID-19 pandemic is ongoing. Getting sick with COVID-19 can impact your health. It can also cause death.
It is important to remember there will always be new variants of the virus that causes COVID-19 infection. But we have tools and the resources to protect ourselves and our loved ones from severe symptoms. The best thing you can do to protect yourself and your community is a multi-step approach that includes:
- Staying up to date with your COVID-19 vaccine
- Wearing a well-fitted N95, KN95, or KN94 mask in public indoor spaces
- Improving indoor air quality through adequate ventilation and filtration
What Is COVID-19 (Coronavirus Disease)?
COVID-19 is a disease caused by the virus SARS-CoV-2. COVID-19 affects many different parts of the body, including the lungs, stomach, heart, blood vessels, and brain. COVID-19 is primarily a respiratory system (breathing) disease, but experts believe it can also affect the vascular (blood vessel) and neurologic (nervous system) systems.
The virus spreads easily and quickly through the air. A person with the virus can spread it to other people by talking, coughing, sneezing, singing, or breathing. The virus is carried by large or small droplets that are expelled from (breathed out) the mouth or nose out into the air. Very small droplets can spread in the air. The virus can spread even if a person doesn’t have symptoms. The virus spreads most easily in indoor spaces with poor air ventilation.
What Are the Symptoms of COVID-19?
COVID-19 symptoms can feel like a cold, the flu, or pneumonia. Some people may have mild symptoms, while some may have complications – serious health issues like severe pneumonia – which can lead to death.
According to the Centers for Disease Control and Prevention (CDC), common COVID-19 symptoms can include:
- Fever
- Chills
- Cough
- Shortness of breath or trouble breathing
- Feeling tired and weak – more than usual
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Stuffy or runny nose
- Diarrhea
- Nausea or vomiting
If you have these emergency warning signs, call 911 or go to the emergency room right away:
- Trouble breathing or shortness of breath
- Pain or pressure in the chest that doesn’t go away
- New and sudden confusion
- Can’t wake up or stay awake
- Cyanosis – tissue color changes on mucus membranes (like tongue, lips, and around the eyes) and fingertips or nail beds – the color appears grayish or whitish on darker skin tones and bluish on lighter skin tones
This list may not include all symptoms. Symptoms may appear 2 to 14 days after coming in contact with the virus. If you have any symptoms that are severe or concerning, call your doctor.
What Should I Do If I Think I Have COVID-19?
Continue to take your asthma and allergy medicines at the first sign of symptoms as listed on your Asthma Action Plan. Keep taking these medicines as prescribed:
- Quick-relief medicine (such as albuterol)
- Inhaled corticosteroids (controller medicines)
- Oral corticosteroids (such as prednisone)
- Biologics
- Antihistamines (allergy medicine)
- Proton pump inhibitors for acid reflux
- Nasal allergy sprays
- Allergy immunotherapy
If you have any questions about asthma medicines and COVID-19, talk with your health care provider.
If you have symptoms and think you may have COVID-19, you may want to take a COVID-19 test. There are many ways to get tested.
- You can order free at home tests. At the end of Sept. 2024, each U.S. household can order 4 free COVID-19 tests through COVIDTests.gov and they will be mailed to your home. You can sign up for yours today. You can also buy an at home test at any pharmacy and many retail stores.
- Check with your local health department, pharmacy, or community health center as they may also offer free testing. If you feel you need to be seen in clinic, call your doctor to schedule an appointment or go to your nearest urgent care center for a test.
- If you need help getting information or finding testing locations, the disability information and access line can help with any questions you may have.
After you take a test and get your results, take steps to prevent the spread of COVID-19.
- If your test was positive, wash your hands often, wear a mask, and stay home if you are sick. Pay attention to your symptoms, and if they get worse, call your doctor and get emergency care right away. Get plenty of rest and continue to take your asthma medicines as prescribed by your health care provider.
- If you tested negative for COVID-19 and have symptoms, you may have tested before the virus could be detected by the test. In this case, follow the FDA recommendations for testing again. If you continue to test negative for COVID-19, you may have another viral infection or illness. Continue to take actions to prevent the spread of respiratory illnesses by staying home if you are sick and wearing a mask. Contact your doctor if your symptoms get worse or do not go away.
There are treatments available that may be used to treat people who are at risk of severe COVID-19 or complications from COVID-19 and have tested positive for COVID-19. These treatments include antihistamines, acetaminophen, and antiviral medicines such as Paxlovid, Veklury, and Lagevrio. If you are at risk of complications or are more likely to get very sick, contact your doctor and ask about COVID-19 treatments.
- It is important that you contact your doctor right away if you test positive for COVID-19. If prescribed by your doctor, start antiviral medicines as soon as possible, within 5 to 7 days when the symptoms start.
- If you have a weakened immune system, it is important to remember to get plenty of rest. It may take longer for your body to recover from symptoms, and you may even have COVID-19 symptoms longer and more severely than other people. If this happens, call your doctor. There may be additional treatments you can take to feel better and recover.
- Continue to take your medicines as prescribed by your health care provider, drink plenty of fluids, and allow your body to get plenty of rest, even after you start to feel better.
What Happens If I Get COVID-19 and I Have Moderate to Severe Asthma or I Am Immunocompromised?
If you have moderate to severe asthma or a chronic lung disease, you may be more likely to get very sick from COVID-19 or be sicker for a longer period of time. It is important to keep your asthma well-controlled. If your asthma is not controlled, you might be at a higher risk of getting very sick from COVID-19.
If you get COVID-19 or think you might have COVID-19, contact your doctor right away. There are antiviral treatments that may reduce the severity of your illness if you take it within 5 days of having symptoms.
You can be immunocompromised (have a weakened immune system) due to a medical condition, such as another chronic lung disease or from taking immunosuppressive medicines like high-dose oral corticosteroids (20 mg or more of prednisone or equivalent per day for 2 weeks or longer).
If you get very sick from COVID-19, you are more likely to:
- Need to be in the hospital for special care
- Require a ventilator (breathing machine) to help you breathe
- Need intensive care
If you have moderate to severe asthma or are immunocompromised, get the COVID-19 vaccine and follow the multi-steps of protection listed in the section above titled, “How Can I Protect Myself and Other People From COVID-19?”
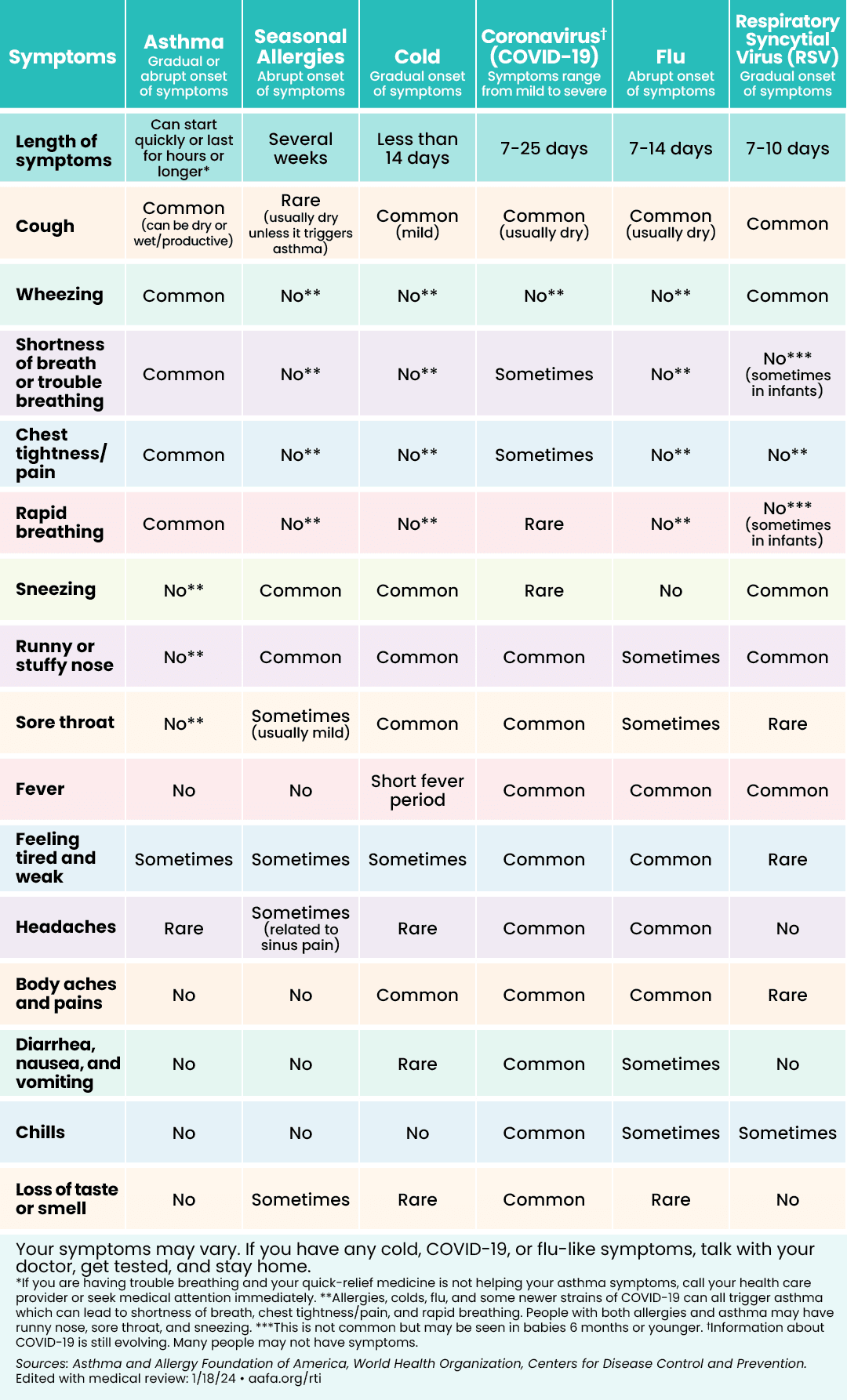
How Can I Tell the Difference Between Asthma, Seasonal Allergies, a Cold, COVID-19, the Flu, a Cold, or RSV?
Some diseases or illnesses have similar symptoms to COVID-19. The charts below can help you figure out if you may be feeling symptoms of asthma, allergies, or a respiratory illness like COVID-19, the flu, a cold, or respiratory syncytial virus (RSV). If you have a fever and a cough, call your doctor right away. If you have seasonal allergies, there are things you can do to treat them at home.
 | 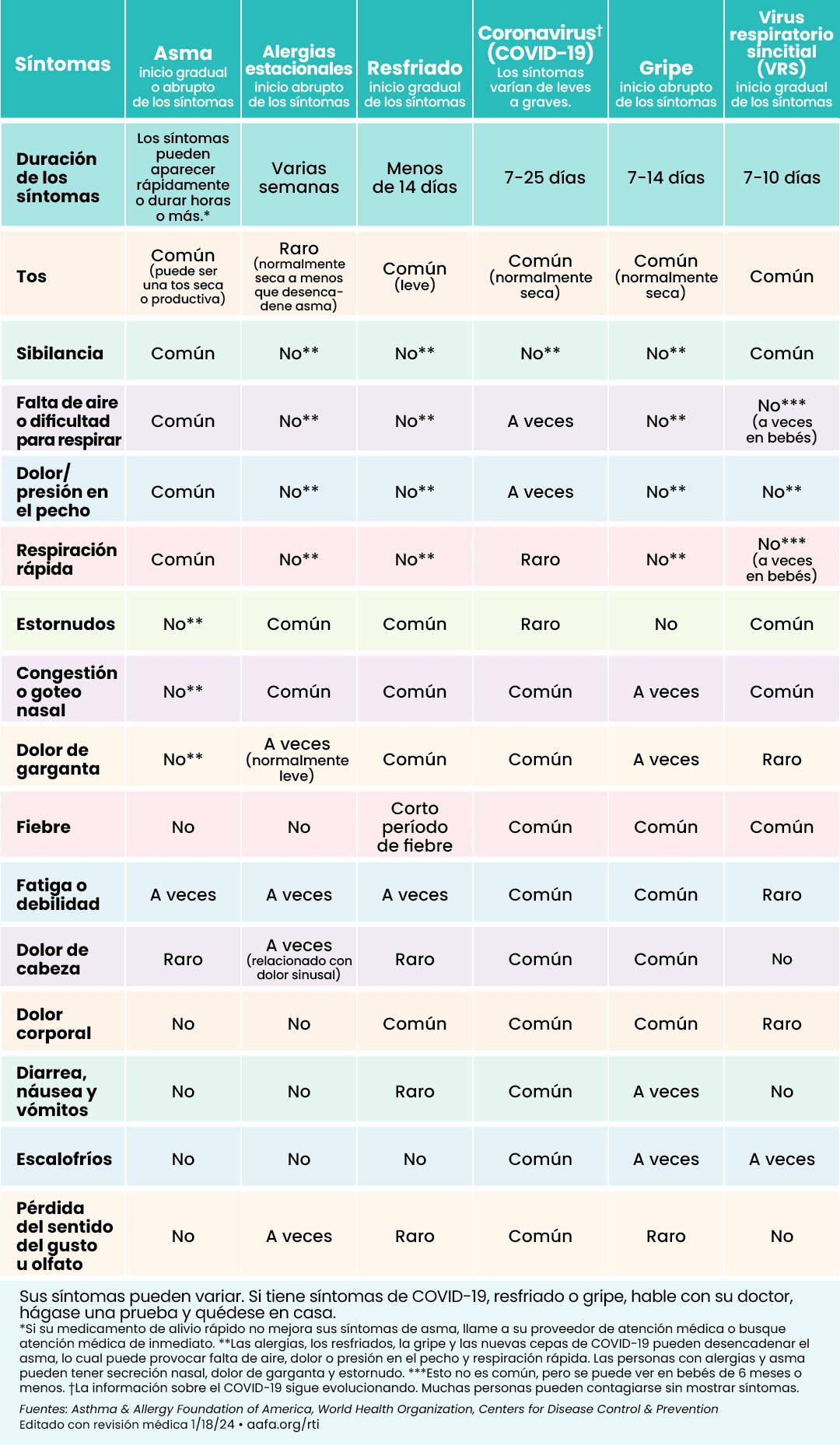 |
Click to see larger image (English) | Click to see larger image (Spanish) |
What Do People with Asthma Need to Know About COVID-19?
Many studies show that having asthma does not put you at a greater risk of getting COVID-19 or having severe COVID-19.1,2,3 But COVID-19 can cause asthma episodes like other respiratory illnesses, such as the flu and RSV, can.
The CDC lists moderate to severe asthma as a chronic lung disease that can make you more likely to have severe illness from COVID-19.
It is important to keep your asthma under control. If your asthma is not under control, you are at a greater risk in general of having an asthma episode or attack, going to the emergency room, staying in the hospital, or even death. If you feel like your asthma is not under control, talk with your doctor as soon as possible.
Should I Keep Taking My Asthma Medicine If I Get COVID-19?
Medicines you may take for asthma and allergies will help you keep your asthma under control. You are at greater risk of having an asthma attack if you stop taking your medicines.
Take your medicines at the first sign of symptoms as listed on your Asthma Action Plan. Keep taking these medicines as prescribed:
- Quick-relief medicine (such as albuterol)
- Inhaled corticosteroids (controller medicines)
- Oral corticosteroids (such as prednisone)
- Biologics
- Antihistamines (allergy medicine)
- Proton pump inhibitors for acid reflux
- Nasal allergy sprays
- Allergy immunotherapy
If you have any questions about asthma medicines and COVID-19, talk with your doctor.
If you have COVID-19 or have been exposed to it and need to take quick-relief medicine (such as albuterol) for an asthma episode, use an inhaler (with a spacer if directed by your doctor) if possible. Using a nebulizer can increase the risk of sending virus particles in the air if you are sick. If you have a nebulizer and solution, it is OK to use it to treat an asthma episode. But when using a nebulizer, limit the number of people in the room or use it in a room by yourself.
How Can I Protect Myself and Other People From COVID-19?
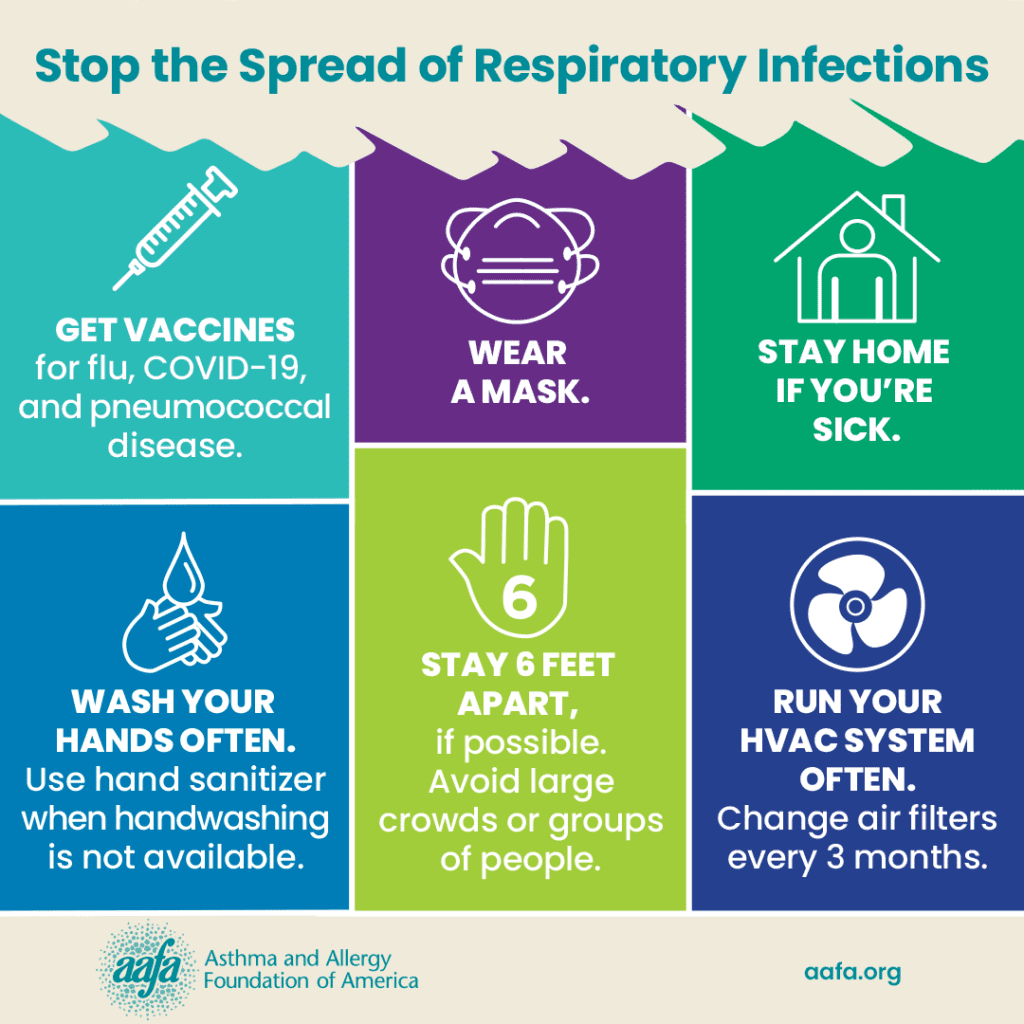
A multi-step approach is best to protect yourself and other people from COVID-19 and other respiratory illnesses:
1. Get an updated COVID-19 vaccine: The vaccine reduces your chance of getting seriously ill, needing hospital care, or dying from COVID-19. The vaccine can also lower your chance of getting Long COVID. The COVID-19 vaccines are now just like a flu vaccine – you get 1 every year. (Some people may need to get more than 1.)
Even if you have already had COVD-19, you should get an updated vaccine. There are new versions of the virus every year and a yearly updated vaccine will better protect you against the latest virus that is going around.
If you recently had COVID-19, you may be able to wait 3 months before getting your COVID-19 vaccine dose.

2. Avoid close contact with sick people: The more you are around people who have COVID-19 or other respiratory illnesses, you will have a greater chance of getting sick. Avoid crowded rooms or buildings when possible, but especially during times when respiratory illnesses are spiking in your community.
3. Wear a tight-fitting mask: Masks and respirators help stop viruses from spreading from person to person. Wear an N95 mask that fits well for the most protection. Wearing a mask is especially helpful in crowded indoor spaces or spaces that don’t have good ventilation (air flow). In general, you do not need to wear a mask in outdoor settings unless you are at a crowded outdoor event (like a concert) during a time of high numbers of COVID-19 cases.
4. Improve ventilation: Open windows, change air filters, use air cleaners, and run fans to improve air flow in your home, school, or workspace. This will help lower the volume of virus particles in your indoor air.
5. Stay home when you are sick: COVID-19, as well as many other respiratory illnesses, can easily spread to others. If you are sick or have symptoms, stay home, get tested, and talk with your health care provider.
6. Wash your hands: When you cough or sneeze into your hand, you can spread viruses to the next item or person you touch. Wash your hands often to prevent illnesses such as the flu and common cold.
7. Cover your cough and sneeze: If you are sick, you can spread your illness. Protect other people by wearing a mask. If you do not have a mask on, cover your cough and sneeze with tissue, or by coughing into your elbow.
Where Can I Get the COVID-19 Vaccine?
You can get the COVID-19 vaccine at most drug stores in the United States. Your local health department or health care provider may also offer vaccines. To find where you can get a COVID-19 vaccine near you, visit: Vaccines.gov
Why Do the COVID-19 Vaccines Keep Changing? If I Get One Vaccine, Why Doesn’t It Last Forever?
The COVID-19 vaccine protects against severe illness, hospital stays, and even death. Viruses are constantly changing, so the experts who make vaccines have to change the vaccines to be more effective.
This does not mean the vaccines are not working. They are. Your protection goes down over time after you get a shot, especially if you are at high risk for severe illness from COVID-19. This is why it’s important to get the updated vaccine when it is available.
What Is Long COVID and What Do I Do If I Think I Have It?
Long COVID, or post COVID conditions, refers to signs, symptoms, and conditions that may develop after you have COVID-19. Many people who get COVID-19 get better after a couple of weeks. For some, it may take 4 weeks or longer. Long COVID shows up at least 4 weeks after you get COVID-19.
Long COVID includes symptoms that can last 3 months or longer. They may even be ongoing. These symptoms may be mild to severe. They may also go away and then come back over weeks and months.
You are at higher risk of getting Long COVID if you:
- Had a more severe form of COVID-19 illness
- Have underlying health conditions and are age 65 or older
- Did not get a COVID-19 vaccine
There is no test to tell if you have Long COVID. Long COVID can last for weeks, months, and sometimes years. Talk with your doctor if your symptoms last longer than 4 weeks.
Long COVID is a serious condition. For some people, it can greatly affect their quality of life. Some symptoms can even cause other health issues that may result in disability. Long COVID may be considered a disability under the Americans with Disabilities Act (ADA) if your symptoms greatly limit one or more major life activity.4
Medical Review: September 2024 by Neeta Ogden, MD
Closed
References
- Chhiba, K.D., Patel, G.B., Vu, T.H.T, Chen, M.M., Guo, A., Kudlaty, E., Mai, Q., Yeh, C., Muhammad, L.N., Harris, K.E., Bochner, B.S., Grammar, L.C., Greenberger, P.A., Kalhan, R., Kuang, F.L., Saltoun, C.A., Schleimer, R.P., Stevens, W.W., & Peters, A.T. (2020). Prevalence and characterization of asthma in hospitalized and non-hospitalized patients with COVID-19. Journal of Allergy and Clinical Immunology. https://doi.org/10.1016/j.jaci.2020.06.010
- Butler, M. W., O’Reilly, A., Dunican, E. M., Mallon, P., Feeney, E. R., Keane, M. P., & McCarthy, C. (2020). Prevalence of comorbid asthma in COVID-19 patients. Journal of Allergy and Clinical Immunology. https://doi.org/10.1016/j.jaci.2020.04.061
- Lieberman-Cribbin, W., Rapp, J., Alpert, N., Tuminello, S., & Taioli, E. (2020). The Impact of Asthma on Mortality in Patients With COVID-19. Chest. https://doi.org/10.1016/j.chest.2020.0air pol.575
- Guidance on “Long COVID” as a Disability Under the ADA, Section 504, and Section 1557. (2021, July 26). HHS.gov; Office for Civil Rights (OCR). https://www.hhs.gov/civil-rights/for-providers/civil-rights-covid19/guidance-long-covid-disability/