Asthma Symptoms
Asthma Signs and Symptoms
When you have asthma, it’s important to know what is happening in your airways, as well as common asthma symptoms. Understanding asthma symptoms can help you know what your triggers are, when you need quick-relief (“rescue”) medicines, and when you are having a medical emergency.
There are three changes in your airways when you have asthma:
- Swelling inside the airways
- Excess mucus clogs the airways
- Muscles tighten and squeeze around the airways
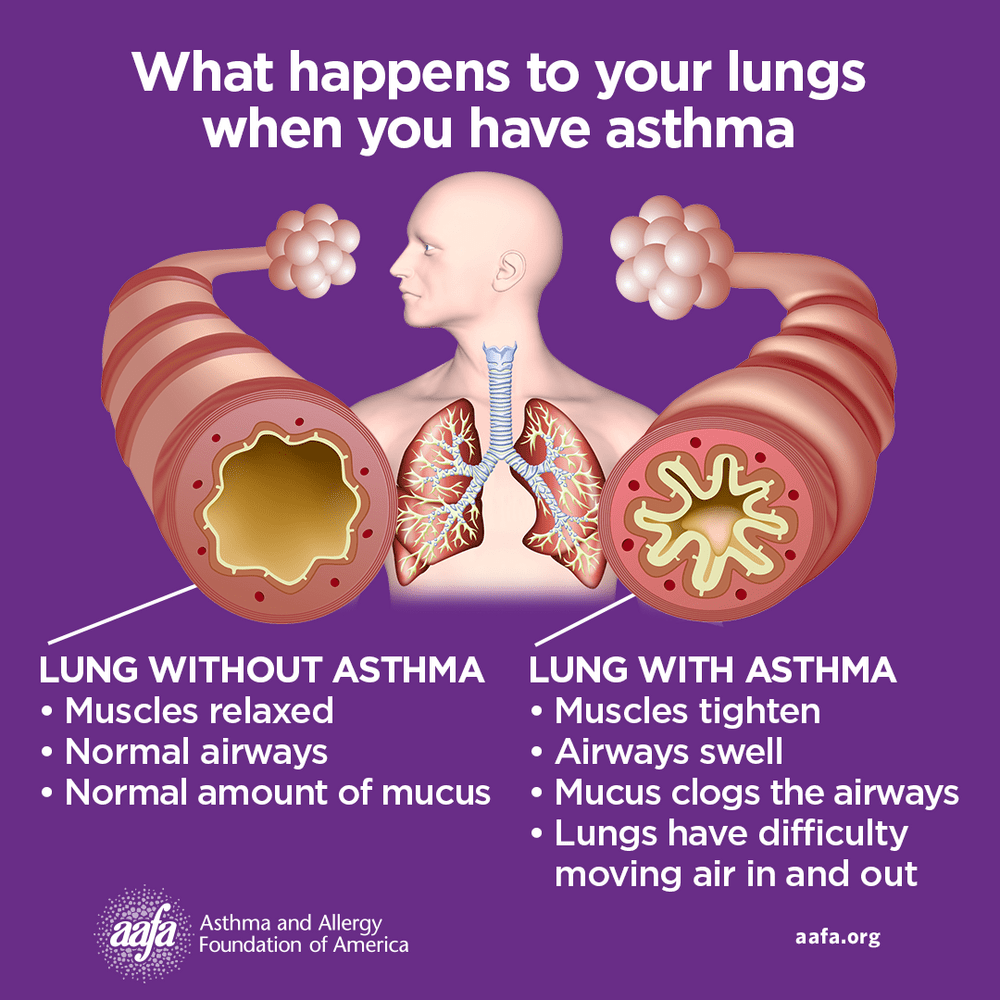
This swelling, clogging, and muscle tightening makes your airways smaller or narrower. This makes it harder for air to flow easily through your airways, and it becomes harder to breathe. This causes asthma symptoms, also known as an asthma episode, flare-up, or attack. It can happen at any time. Mild symptoms may only last a few minutes while more severe asthma symptoms can last hours or days.
Breathing becomes difficult and stressful, like trying to breathe through a straw stuffed with cotton.
Common signs and symptoms of asthma include:
- Shortness of breath
- Cough
- Chest tightness or pain
- Wheeze (a whistling sound when you breathe)
- Waking at night due to asthma symptoms
- A drop in your peak flow meter reading (if you use one)
Not everyone with asthma has the same symptoms. You may only have one symptom, or you may have many symptoms.
closed
What Are the Signs and Symptoms of an Asthma Episode or Attack?
If you have asthma, work with your doctor to make an Asthma Action Plan. An Asthma Action Plan is a document that tells you how to manage your asthma according to your symptoms.
Talk with your doctor about your symptoms and steps to manage them. If you do not have an Asthma Action Plan, you can download and email AAFA’s Asthma Action Plan (available in English and Spanish) to your doctor or print a copy for your doctor to fill out.
Take your asthma medicines as directed on your Asthma Action Plan, and always take your quick-relief medicines at the first sign of symptoms.
An asthma action plan has three zones:
![]() Asthma Green/Go Zone
Asthma Green/Go Zone
Take your control or preventive medicines as directed (if prescribed). You are in the Green/Go Zone if you have all of these:
- Breathing is good
- No cough or wheeze
- No chest tightness or pain
- Can sleep through the night
- Can work and play
Green/Go Zone Actions
If exercise is an asthma trigger, your Asthma Action Plan may have you take quick-relief medicine before you exercise to prevent asthma symptoms before you begin (sometimes referred to as “pre-treatment”). This will be listed on the Green/Go Zone of the plan.
When you are in the Green/Go Zone, your asthma is well-controlled.

Asthma Yellow/Caution Zone
You are in the Yellow/Caution Zone when you first start having asthma signs or symptoms. Signs and symptoms that your asthma is getting worse include:
- Shortness of breath
- Cough
- Chest tightness or pain
- Wheezing
- Waking at night due to asthma symptoms
- Having any signs or symptoms after an exposure to a known trigger
- Having breathing difficulty when sick with a cold or respiratory illness
Yellow/Caution Zone Actions
Take your asthma medicines as listed on your Asthma Action Plan at the first sign of symptoms when you are in the Yellow/Caution Zone. This may be one quick-relief medicine (like albuterol), a quick-relief medicine and controller taken one right after each other, or a combination inhaler. Monitor your symptoms until they improve.
If your quick-relief medicines don’t help and your symptoms do not improve, call your doctor.
If you are in the Yellow/Caution Zone two or more times per week, it is a sign your asthma is not controlled and you may need to contact your health care provider (doctor).
 Asthma Red/Danger Zone
Asthma Red/Danger Zone
If you are in the Red/Danger Zone, take your quick-relief medicines. If your breathing does not improve quickly, get emergency help. Severe asthma episodes can be life-threatening.
Signs and symptoms of an asthma emergency that need urgent medical care:
- Asthma is getting worse quickly
- Asthma quick-relief medicines are not helping
- Chest tightness or pain
- Severe shortness of breath
- Breathing is faster or slower than normal
- Breathing may be hard or shallow
- Trouble walking or talking due to shortness of breath
- Chest retractions (skin sucks in between or around the neck, chest plate, and/or rib bones when inhaling; this is rare in adults)
- Ribs or stomach moving in and out deeply and rapidly
- Expanded chest that does not deflate when you exhale
- Shoulders hunched over (“posturing”)
- Cyanosis, a tissue color change on mucus membranes (tongue, lips, and around the eyes) and fingertips or nail beds – the color appears grayish or whitish on darker skin tones and bluish on lighter skin tones
Infants, toddlers, and children may have different asthma emergency signs and symptoms than adults. Signs and symptoms of a severe asthma episode in infants, toddlers, and children:
- Infants with asthma who fail to respond or recognize parents
- Nasal flaring – nostrils open wide/flare (may be rare in adults)
- Working harder to breathe (nasal flaring, skin is sucking in around and between ribs or above the sternum, or exaggerated belly movement or belly breathing)
- Cyanosis, a tissue color change on mucus membranes (tongue, lips, and around the eyes) and fingertips or nail beds – the color appears grayish or whitish on darker skin tones and bluish on lighter skin tones
- Infants with asthma in respiratory distress may have bobbing head, grunting, floppy body, or be irritable, agitated, cranky, and/or lethargic (sluggish)
Red/Danger Zone Actions
Red/Danger Zone symptoms are a medical emergency. Take your quick-relief medicines right away as directed on your Asthma Action Plan and then get immediate medical attention. Call 911 or go directly to the emergency room.
Follow up with your provider within two days of an emergency department visit or hospital stay.
Early Warning Signs of an Asthma Episode or Attack
Sometimes you may have early warning signs that an asthma episode is coming. You may have these signs before you start to have more obvious asthma symptoms. Identifying warning signs and taking steps to prevent asthma episodes can help keep asthma well-controlled. Early warning signs may be different for each person, but some common warning signs can include:
- Increased mucus/sputum production
- Runny/stuffy/congested nose
- Itchy neck or chin
- Feeling tired, weak, or lack of energy
- Raised shoulders, slouching
Your doctor can help you identify your early warning signs. When you have early warning signs, treat this as if you are in the Yellow/Caution Zone. Take your quick-relief asthma medicines as soon as you start to have early warning signs.
How Can I Prevent and Treat Asthma Symptoms?
There is no cure for asthma, but it can be managed. There are two steps to controlling asthma: taking medicines and avoiding or limiting asthma triggers.
To prevent asthma symptoms:
- Avoid or limit contact with your asthma triggers and allergens. Use AAFA’s Healthier Home Checklist to identify asthma triggers and allergens in your home and make your indoor environment healthier.
- Get vaccinated. Respiratory infections like colds and the flu can worsen asthma. Get a flu vaccine every year. Keep your lungs healthy by getting other vaccinations as recommended.
- Create an Asthma Action Plan with your doctor. Follow it when you have symptoms. If you are having trouble staying in the Green/Go Zone, your asthma may not be well-controlled. Talk with your doctor about your treatment plan.
- Take your asthma medicines as directed. If your doctor prescribed a medicine to control your asthma, take it as directed. This may be as needed or every day. Follow your Asthma Action Plan.
- Take care of your general health. It can be hard to take care of your health but doing so can help you better manage asthma. Try to get plenty of sleep and exercise. Eat healthy foods as much as possible, stay hydrated, and find ways to manage stress.
To treat sudden asthma symptoms:
- Take quick-relief medicines at the first sign of symptoms. Always have your quick-relief medicines with you. You never know when or where symptoms will happen. Take quick-relief medicines as soon as you start feeling symptoms.
- Take medicines as directed on your Asthma Action Plan. If your symptoms are not improving or getting worse quickly, seek medical attention right away. This means you are in the Red/Danger Zone.
Talk with your doctor about your asthma symptoms and be sure to discuss any changes in your asthma control. With proper treatment and an asthma management plan, you can reduce your symptoms and enjoy a better quality of life.
How Do I Know If My Asthma Is Not Well-Controlled?
A good way to know if your asthma is not well-controlled is by answering these questions:
- Do you have asthma symptoms more than two times a week?
- Do you take your quick-relief medicine more than two times a week?
- Do you wake up from asthma more than two times a month?
- Do you use oral corticosteroids more than two times a year?
If you answer “yes” to any of these questions, talk with your doctor.
If your asthma is not well-controlled, your daily activities may be limited. You may miss work or school. You may increase your chances of having complications from a respiratory infection. And you may be at greater risk for going to the emergency room, staying in the hospital, or even dying from asthma.
Why Does My Asthma Act Up at Night?
Asthma can get worse at night. If you have symptoms at night, it’s called nighttime asthma. This is often a sign of uncontrolled asthma. It probably has to do with natural body rhythms and changes in your body’s hormones. With the right asthma management and treatment, you should be able to sleep through the night.
What Other Tools Can I Use for Monitoring Asthma Control?
Peak Flow Meter
Sometimes doctors recommend a peak flow meter – a handheld device that measures how well air moves out of your lungs. A peak flow meter, when used every day, can spot reduced airflow before you notice the signs and symptoms of an asthma episode.
Peak flow meter readings can help you monitor your asthma control. But they are just one tool. Your peak flow meter reading is not the only indicator of asthma control. Always follow your Asthma Action Plan.
Pulse Oximeter
Doctors use pulse oximeters (or “pulse ox”) to measure how much oxygen your blood is carrying. Some people with asthma may experience a drop in their oxygen levels in their blood.
Pulse oximeters you can buy online and use at home are not as accurate as medical grade devices. Monitoring your blood oxygen levels with pulse oximeters is not a recommended part of home management of asthma.
Lung Function Tests
Your allergist (allergy and asthma doctor) or pulmonologist (lung doctor) may use different lung function tests to assess your asthma control. Learn more about the tests used to diagnose and monitor asthma.
Asthma Medicines: Control and Quick-Relief or a Combination?
Your provider will prescribe asthma medicines to help you control or prevent symptoms as well as medicines that work to relieve symptoms when they happen. You may be prescribed two separate medicines, or a medicine that combines them into one.
The medicines your doctor prescribes will depend on the severity of your asthma. Follow your Asthma Action Plan to know which medicines to take and when to take them. Your plan may call for:
- An inhaled corticosteroid (ICS) taken daily to control and prevent symptoms plus a quick-relief inhaler (like albuterol) to treat symptoms when they happen
- An ICS inhaler plus a quick-relief inhaler taken as needed, one right after the other, to treat symptoms when they happen
- A combination inhaler that includes both types of medicines (control and quick-relief) into one inhaler that can be used daily and/or as needed
- Only a quick-relief inhaler to treat symptoms when they happen (for intermittent asthma only)
- Adding a biologic medicine (a shot or infusion) to your control and quick-relief medicines
Medical Review July 2021 by Bradley A. Becker, MD, and January 2022 by Mitchell Grayson, MD
Knowing how to manage asthma is important for better health and quality of life. We offer an online course called ASTHMA Care for Adults. This comprehensive program covers a full range of topics everyone with asthma needs to know. This self-paced online course is presented in different formats, such as videos, animations, handouts and more.