Asthma
Respiratory Infections and Asthma
Respiratory infections (also called respiratory illnesses) are caused by viruses or bacteria that make you sick. These infections affect your lungs, nose, sinuses, and throat, especially when you have asthma. They can cause a runny nose, cough, fever, or sore throat.
Respiratory infections are a common asthma trigger, especially in children. People with asthma have swelling, inflammation, and mucus in their airways. And when they get sick, it can be even harder for them to breathe.
- COVID-19 (caused by the SARS-CoV-2 coronavirus)
- Flu (caused by the influenza virus)
- Pneumonia (caused by bacteria, virus, or fungus)
- Respiratory syncytial virus (RSV)
- Whooping cough (pertussis)
- Common cold (caused by more than 200 different viruses)
- Strep (caused by Streptococcus bacteria)
- Croup (caused by parainfluenza virus)
You can have more than one respiratory infection at the same time.
What Are the Symptoms of Respiratory Infections?
Infections can cause a runny nose, fever, or sore throat. They can also cause symptoms, like coughing and shortness of breath, which overlap with asthma. Or sneezing, which also happens with seasonal allergies. Respiratory infections can also make someone’s asthma worse.
AAFA’s respiratory illness symptom chart can help you learn what is similar and what is different between asthma, seasonal allergies, colds, COVID-19, flu, and RSV.
Information is still changing. We will update this chart as new evidence comes out.
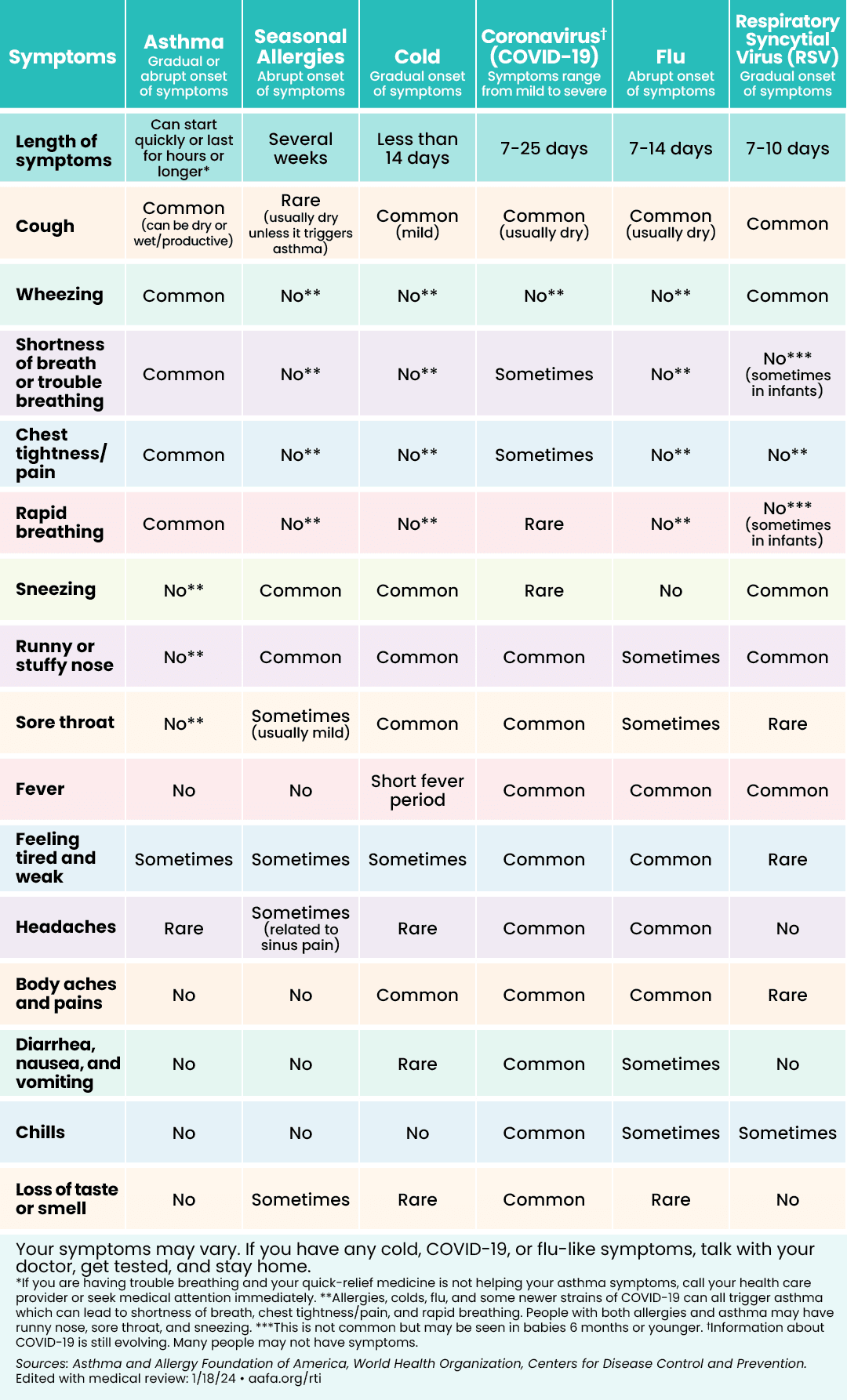 | 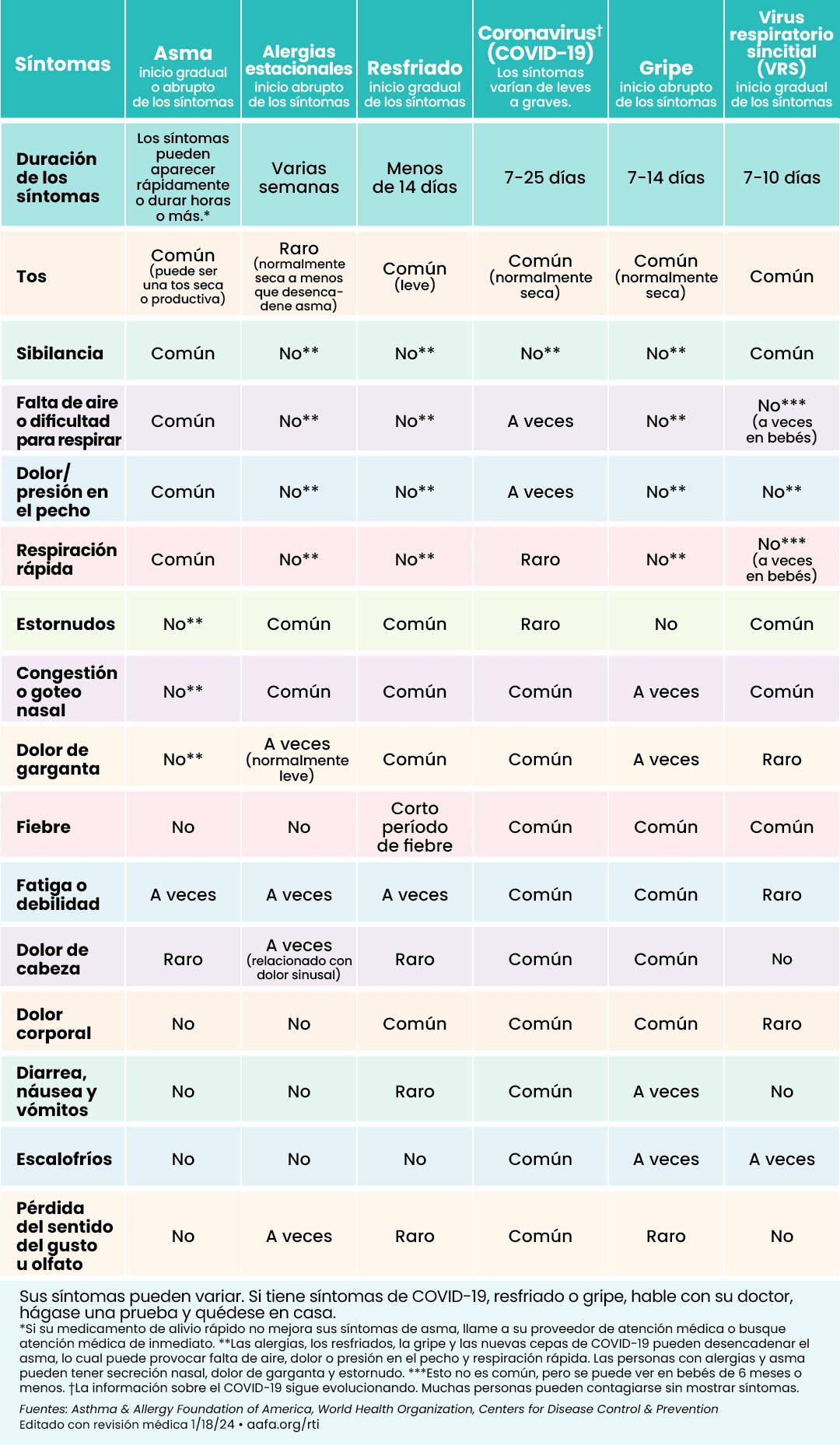 |
Click to see larger image (English) | Click to see larger image (Spanish) |
What Should I Do If I Have a Respiratory Illness?
Follow your Asthma Action Plan. If your Asthma Action Plan doesn’t tell you what to do if you get sick, call your doctor to ask if you should change how you take your prescribed asthma medicine while you are sick. Always keep your quick-relief asthma medicines with you to treat asthma symptoms.
Get tested if you have symptoms of the flu or COVID-19. You can go to your local pharmacy, care clinic, or urgent care. There are also at-home tests available for COVID-19 and the flu. If you have symptoms that are severe or affecting your breathing, contact your doctor right away even if you test negative.
Talk with your doctor about your symptoms. Ask if you can take over-the-counter medicines to reduce some of your symptoms. If you are sick with the flu or COVID-19, ask your doctor about antiviral treatment.
Get medical help right away (or call 911) if you have any of these danger signs:
- Asthma is getting worse quickly
- Asthma quick-relief medicines are not helping
- Chest tightness or pain
- Severe shortness of breath
- Breathing is faster or slower than normal
- Breathing may be hard or shallow
- Trouble walking or talking due to shortness of breath
- Chest retractions (skin sucks in between or around the neck, chest plate, and/or rib bones when inhaling – this is rare in adults)
- Ribs or stomach moving in and out deeply and rapidly
- Expanded chest that does not deflate when you exhale
- Shoulders hunched over (“posturing”)
- Cyanosis, a tissue color change on mucus membranes (tongue, lips, and around the eyes) and fingertips or nail beds – the color appears grayish or whitish on darker skin tones and bluish on lighter skin tones
Infants, toddlers, and children may have different asthma emergency signs and symptoms than adults. Signs and symptoms of a severe asthma episode in infants, toddlers, and children include:
- Infants with asthma who fail to respond or recognize parents
- Nasal flaring – nostrils open wide/flare (may be rare in adults)
- Working harder to breathe (nasal flaring, skin is sucking in around and between ribs or above the sternum, or exaggerated belly movement or belly breathing)
- Cyanosis, a tissue color change on mucus membranes (tongue, lips, and around the eyes) and fingertips or nail beds – the color appears grayish or whitish on darker skin tones and bluish on lighter skin tones
- Infants with asthma in respiratory distress may have a bobbing head, grunting, a floppy body, or be irritable, agitated, cranky, and/or lethargic (sluggish)
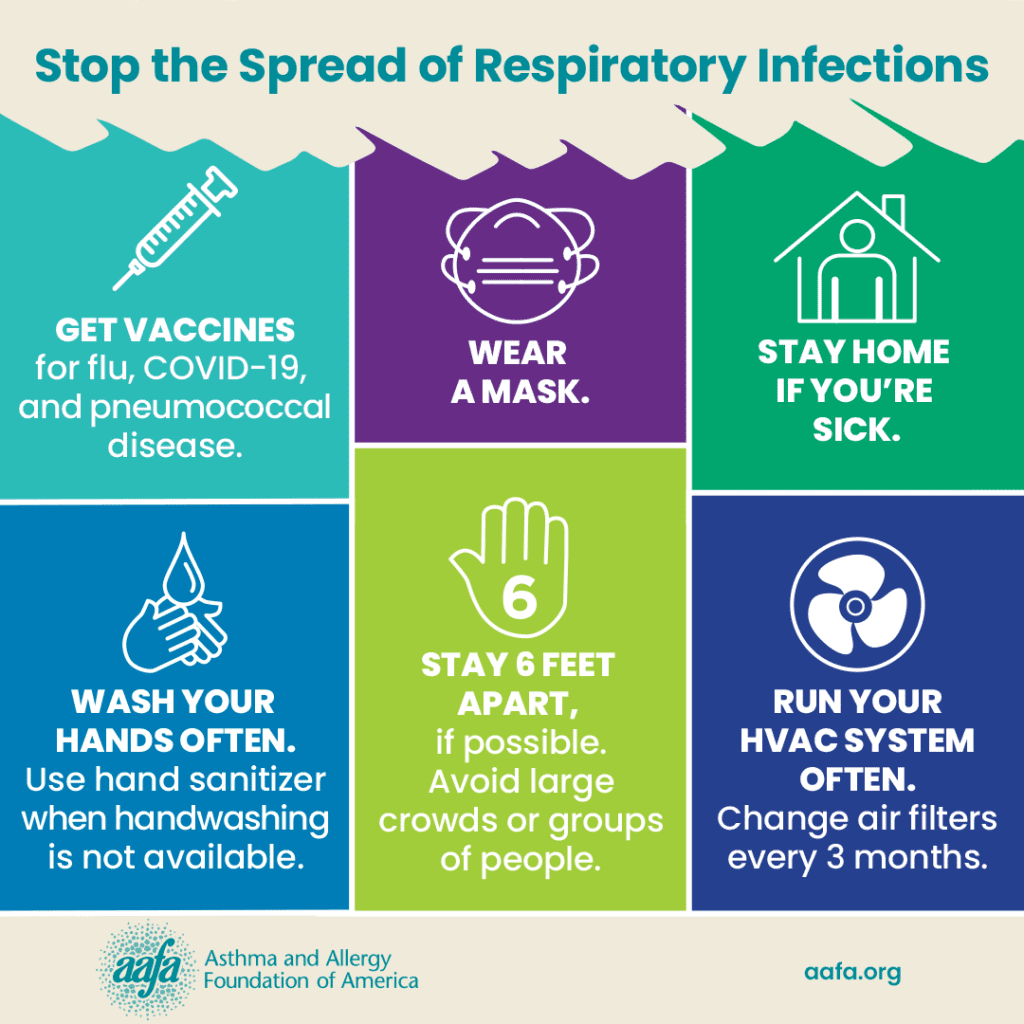
How Can I Prevent Respiratory Illness?
For more information about vaccine recommendations for individuals and families with asthma and allergies, visit: aafa.org/vaccine
Infections like the flu are a major cause of asthma episodes or attacks. And according to the Centers for Disease Control and Prevention (CDC), people with asthma are at higher risk for developing serious complications (like pneumonia) from the flu. Follow these steps to protect yourself and your loved ones from respiratory illnesses:
- Wash your hands often with soap and warm water for 20 seconds, especially after touching frequently used surfaces like doorknobs.
- Avoid touching your eyes, nose, or mouth.
- Get a yearly flu vaccine.
- Get the updated COVID-19 vaccine. These vaccines are now yearly just like the flu.
- Talk with your doctor about getting the pneumococcal [noo-muh-KOK-uhl] vaccine. You should only need the shot once and a booster as needed.
- Stay away from people who are sick. If you have symptoms, stay home.
- Keep your breathing equipment clean. This includes your asthma inhaler, spacer or valved holding chamber, nebulizer and nebulizer tubing, and mouthpiece.
- Do not share your breathing equipment or medicines with others.
- Consider wearing a face mask when in large crowds or in public.
It’s important to always keep your asthma under control. If your asthma is well-controlled when you get sick, you reduce your chances of having an asthma attack, having complications, or staying in the hospital.
Learn More About Your Asthma Medicines
Use our asthma medicine search tool to look up information on specific medicines, prescribing information, and possible side effects
Medical Review: January 2024 by Mitchell Grayson, MD













